
Fibroids (Myomas) are benign tumors originating from the Uterus (uterus) tissue, the diameter of which is usually from 1-2 cm to 10-15 cm. Fibroids are sometimes described by the physicians as fibroids, leiomyomas, or fibromyomas. They are quite common in women. Usually, fibroids that are small and do not cause complaints are only followed by the gynecologists. Since the hormone estrogen causes the growth of fibroids, they increase in size during pregnancy, while they shrink and calcify after menopause. Fibroids are of three types depending on where they are in the uterus, which we call the uterus.
Submucous fibroids: Those in the innermost part of the uterus
Intramural fibroids: Those located inside the uterine tissue, that is, the muscle tissue. (The most common type)
Subserous fibroids: These are fibroids that grow out of the uterine tissue.
Submucous and intramural fibroids mostly cause complaints such as prolonged and heavy menstrual bleeding. In large intramural fibroids and sub serosal fibroids with mass effect, symptoms such as abdominal pain, back and leg pain, feeling of fullness, pain with sexual intercourse, frequent urination due to bladder compression are encountered. Myomas that cause complaints need to be treated and non-surgical myoma treatment can be applied to many myomas.
WHAT ARE THE CLASSICAL TREATMENTS FOR FIBROIDS?
 The most used classical methods in the treatment of fibroids are hysterectomy and myomectomy. Obstetricians perform these two operations. Non-surgical treatment methods in myoma treatment are fibroid embolization, RF ablation and HIFU (High Intensity Focused Ultrasound). Interventional radiologists apply these modern treatment methods. Modern non-surgical treatment methods should be preferred as much as possible because they are easier and less side-effects treatments, because hysterectomy operation means irreversible removal of the uterus. Your obstetrician and the interventional radiologist who performs these treatments should decide between them which treatment would be more appropriate for you. If you have been offered a direct hysterectomy operation, it would be beneficial to see an interventional radiologist experienced in non-surgical fibroid treatment before removing your uterus.
The most used classical methods in the treatment of fibroids are hysterectomy and myomectomy. Obstetricians perform these two operations. Non-surgical treatment methods in myoma treatment are fibroid embolization, RF ablation and HIFU (High Intensity Focused Ultrasound). Interventional radiologists apply these modern treatment methods. Modern non-surgical treatment methods should be preferred as much as possible because they are easier and less side-effects treatments, because hysterectomy operation means irreversible removal of the uterus. Your obstetrician and the interventional radiologist who performs these treatments should decide between them which treatment would be more appropriate for you. If you have been offered a direct hysterectomy operation, it would be beneficial to see an interventional radiologist experienced in non-surgical fibroid treatment before removing your uterus.
Hysterectomy operation is a widely applied treatment, although it has many negative consequences on quality of life. The most important reason behind the prevalence of this treatment is that the uterus is seen as an organ that only serves to give birth to a baby. Another reason is that cancers that may develop due to the uterus and ovaries, which do not function much after a certain age, are prevented. There are a considerable number of scientists and physicians who oppose these two views.
After hysterectomy, that is, complete removal of the uterus, results that seriously reduce the quality of life of patients may occur. First, let us talk about the idea of preventing cancer by removing these organs. While a woman’s risk of dying from uterine or ovarian cancer is less than 1%, the risk of dying from cardiovascular disease is around 50%. There are studies showing that the risk of heart attack increases three times after removal of the uterus. How accurate can it be to ignore the risk of death from such a frequent disease? In addition, the risk of osteoporosis increases after hysterectomy. If the ovaries are removed along with the uterus, the risk of osteoporosis (bone loss) increases even more. Hormone pills given to avoid these negative consequences also cause some separate risks. For example, women using combined estrogen-progesterone pills have been found to have a slight increase in the incidence of heart disease, thromboembolism (clot formation in the veins and lung cancer) and breast cancer. For these reasons, it is recommended to use these hormones for a brief time. In the light of all this information, it can be said that if there is no cancer in the uterus and ovaries, it is of great benefit to avoid unnecessary hysterectomy and oophorectomy operations.
In some studies, it has been shown that 30% of women experience symptoms such as frequent urination, constant urination, and urinary incontinence after removal of the uterus. These problems can be serious enough to require surgical intervention. The most important reason for this is the cutting of the thin nerves of the bladder during the surgery. Cystocele (sagging in the bladder) due to the collapse of the anterior wall of the vagina and rectocele (prolapse of the large intestine into the vagina) due to the collapse of the posterior wall of the vagina can be seen. In addition, after the removal of the uterus, the rectum, which is the last part of the large intestine, may sag in its position and cause constipation-like complaints.
Myomectomy is one of the classically performed operations. In this operation, only the fibroids are removed, and the uterus is not removed. However, this is not so easy when there are many fibroids. The higher the number of fibroids, the more difficult it is to remove all the fibroids, the greater the blood loss and other complications associated with myomectomy operation, and the greater the risk of the operation turning into a hysterectomy. In addition, when there are many fibroids, it becomes impossible to determine which fibroid is the cause of the main complaints. In this case, the success chance of myomectomy operation decreases, and the second operation is usually hysterectomy when the complaints do not resolve after myomectomy. However, in such patients, all fibroids can be effectively treated without removal of the uterus with fibroid embolization therapy. Embolization should be the first treatment method of choice in patients with multiple uterine fibroids. To understand the advantages of non-surgical myoma treatment with modern methods and which treatment option is more suitable for you, it is useful to consult an interventional radiologist who applies these treatments.
EVALUATION BEFORE NON-SURGICAL TREATMENT (EMBOLIZATION)

Contrast-enhanced Pelvic MRI should be performed before fibroid embolization or other non-surgical fibroid treatments. Ultrasound alone is not sufficient for the selection of uterine fibroid treatment. Since the number, shape, location, and viability of fibroids can be evaluated in detail in MRI, pelvic MRI is particularly important in choosing the right treatment method. Non-surgical myoma treatment can be offered as a primary choice for all fibroids that do not have thin stems and have intense blood flow in MRI examination. Non-surgical fibroid treatment can also be used as a single session in exceptionally large fibroids to reduce preoperatively. However, with embolization treatments performed by an experienced interventional radiologist, treatment can usually be provided without the need for surgery.
NON-SURGICAL FIBROID TREATMENTS (EMBOLIZATION, RF ABLATION, HIFU)
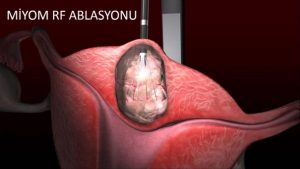
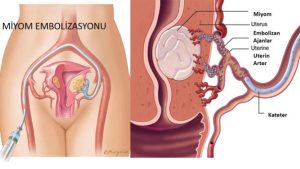
In non-surgical fibroid treatments, if there is only one dominant fibroid, which is a rare condition. RF ablation or HIFU (High Intensity Focused Ultrasound) can be chosen as the treatment method. If the fibroid is exceptionally large and has a large blood supply, embolization treatment is preferred. Embolization is recommended as the first choice in cases where there are many fibroids. Although non-surgical uterine fibroid treatments, especially Myoma Embolization, is a well-established treatment protocol applied to thirty thousand women a year in America, it is not a widely heard treatment method in our country. The main reason for this is that there are very few interventional radiologists who can apply this modern treatment method in our country, and the second reason is that it is a treatment method that even obstetricians do not know much about yet. If you have been offered myomectomy treatment and the risk of hysterectomy is mentioned, you should ask your doctor for information about myomectomy embolization treatment.
WHICH TREATMENT IS MORE EFFECTIVE?

First, let us state that hysterectomy surgery, that is, removal of the uterus, should be applied as the last option if it is necessary after all options have been evaluated. We have two options in the treatment of myoma. It is a myomectomy operation where only the fibroid is removed, and fibroid embolization, which is the treatment of fibroids where the vessels feeding the fibroids in the uterus are blocked and the fibroids are killed and reduced.
What are the types of fibroids in which myomectomy operation can be preferred first?
We talked about the types and locations of fibroids in the section on what to know about fibroids. If submucous myoma growing into the uterus and subserous fibroids growing out of the uterus are thin stemmed, they may break off after embolization treatment and fall into the uterus or abdominal cavity and cause distress. Myomectomy should be the first choice in fibroids with such a thin stem.
What are the types of fibroids in which myomectomy operation or non-surgical treatments such as fibroid embolization can be preferred?
If there is only one fibroid, both myomectomy and fibroid embolization can be preferred because it is easy to operate. Even if these fibroids are on the anterior wall, RF ablation treatment can be easily applied. In RF ablation, the fibroid is entered into the fibroid with the help of a needle through the skin and the effect of heat can be treated under local anesthesia. HIFU, which is a rarely used method for a single fibroid, is also among the options. HIFU means high.
Finally, if our patient wants to give birth, myomectomy and embolization treatment carry a similar risk in terms of fertility. It is necessary to choose according to the number and structure of myoma.
What are the types of fibroids in which non-surgical treatments such as fibroid embolization can be preferred?
If the number of fibroids is more than one or even if it covers the entire myometrium, fibroid embolization should be preferred first. Since embolization treatment delivers occlusive particles to all fibroids with high vascularity, treatment for all fibroids is possible in a single session. In fibroid embolization, the uterine tissue is preserved because it is vascularized from other sources. After embolization, all fibroids are observed as dead tissue, while the uterine tissue is observed live in the control MR examination.
Especially large fibroids carry a significant risk for surgery because they have too much blood. Such cases are most likely to go to hysterectomy. Our pre-operative colleagues specifically point out this possibility. In this way, embolization is the first choice for large and excessively bloody fibroids. It is also possible for the fibroids, whose size and blood supply decrease after fibroid embolization, to go to myomectomy operation without any risk. We call these treatments as combined treatments. (First embolization, then myomectomy). Combined therapy should be considered when embolization alone is not sufficient for large fibroids.
ADENOMYOSIS AND NON-SURGICAL TREATMENTS

In the uterus, apart from fibroids, there is another condition called adenomyosis. Among the most important findings in adenomyosis are increased menstrual bleeding, painful menstruation, and pain during sexual intercourse. These findings may also be accompanied by infertility. However, these complaints can also be seen in fibroids and endometriosis. Contrast-enhanced Pelvic MRI should be performed to differentiate adenomyosis and fibroids.
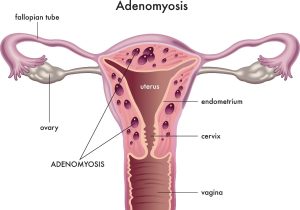
If adenomyosis does not cause serious discomfort to the patient, no treatment is required. However, since patients often have complaints, treatment is often required. The classical treatment of adenomyosis is hormonal spirals and other hormonal drugs. It is especially used to reduce bleeding complaints, but drug treatment is not always successful. It is not possible to completely remove the adenomyosis tissue, especially in diffuse adenomyosis cases, as in myoma surgery. Therefore, if surgical treatment is to be performed in adenomyosis, removal of the entire uterus (hysterectomy) is preferred. Since hysterectomy operation, that is, removal of the uterus, is a treatment option that is not preferred by patients and there are many risks after the operation, embolization treatment is applied in these patients. In scientific studies conducted with a large patient population, it has been determined that approximately 80% of the patients have completely disappeared after embolization.
WHAT ARE THE DISADVANTAGES OF HYSTERECTOMY?

The most used classical methods in the treatment of fibroids are hysterectomy and myomectomy. Obstetricians perform these two operations. Modern non-surgical treatment methods should be preferred as much as possible because they are easier and less side-effects treatments, because hysterectomy operation means irreversible removal of the uterus. Your obstetrician and the interventional radiologist who performs these treatments should decide between them which treatment would be more appropriate for you. If you have been offered a direct hysterectomy operation, it would be beneficial to see an interventional radiologist experienced in non-surgical fibroid treatment before removing your uterus.
Hysterectomy operation is a widely applied treatment, although it has many negative consequences on quality of life. The most important reason behind the prevalence of this treatment is that the uterus is seen as an organ that only serves to give birth to a baby. Another reason is that cancers that may develop due to the uterus and ovaries, which do not function much after a certain age, are prevented. There are a considerable number of scientists and physicians who oppose these two views.

After hysterectomy, that is, complete removal of the uterus, results that seriously reduce the quality of life of patients may occur. First, let us talk about the idea of preventing cancer by removing these organs. While a woman’s risk of dying from uterine or ovarian cancer is less than 1%, the risk of dying from cardiovascular disease is around 50%. There are studies showing that the risk of heart attack increases three times after removal of the uterus. How accurate can it be to ignore the risk of death from such a frequent disease? In addition, the risk of osteoporosis increases after hysterectomy. If the ovaries are removed along with the uterus, the risk of osteoporosis (bone loss) increases even more. Hormone pills given to avoid these negative consequences also cause some separate risks. For example, women using combined estrogen-progesterone pills have been found to have a slight increase in the incidence of heart disease, thromboembolism (clot formation in the veins and lung cancer) and breast cancer. For these reasons, it is recommended to use these hormones for a brief time. In the light of all this information, it can be said that if there is no cancer in the uterus and ovaries, it is of great benefit to avoid unnecessary hysterectomy and oophorectomy operations.
In some studies, it has been shown that 30% of women experience symptoms such as frequent urination, constant urination, and urinary incontinence after removal of the uterus. These problems can be serious enough to require surgical intervention. The most important reason for this is the cutting of the thin nerves of the bladder during the surgery. Cystocele (sagging in the bladder) due to the collapse of the anterior wall of the vagina and rectocele (prolapse of the large intestine into the vagina) due to the collapse of the posterior wall of the vagina can be seen.
In addition, after the removal of the uterus, the rectum, which is the last part of the large intestine, may sag in its position and cause constipation-like complaints.
WHAT ARE THE DISADVANTAGES OF OOPHERECTOMY (OVARY REMOVAL)?

After hysterectomy, that is, complete removal of the uterus, results that seriously reduce the quality of life of patients may occur. First, let us talk about the idea of preventing cancer by removing these organs. While a woman’s risk of dying from uterine or ovarian cancer is less than 1%, the risk of dying from cardiovascular disease is around 50%. There are studies showing that the risk of heart attack increases three times after removal of the uterus. How accurate can it be to ignore the risk of death from such a frequent disease? In addition, the risk of osteoporosis increases after hysterectomy. If the ovaries are removed together with the uterus (oophorectomy), the risk of osteoporosis (bone loss) increases even more. Hormone pills given to avoid these negative consequences also cause some separate risks. For example, women using combined estrogen-progesterone pills have been found to have a slight increase in the incidence of heart disease, thromboembolism (clot formation in the veins and lung cancer) and breast cancer. For these reasons, it is recommended to use these hormones for a brief time. In the light of all this information, it can be said that if there is no cancer in the uterus and ovaries, it is of great benefit to avoid unnecessary hysterectomy and oophorectomy operations.
